asahi.com
Clustered Story
iPS cell - based treatment to debut as early as this summer | The Asahi Shimbun : Breaking News , Japan News and Analysis
asahi.com · Feb 20, 2026 · Collected from GDELT
Summary
Published: 20260220T114500Z
Full Article
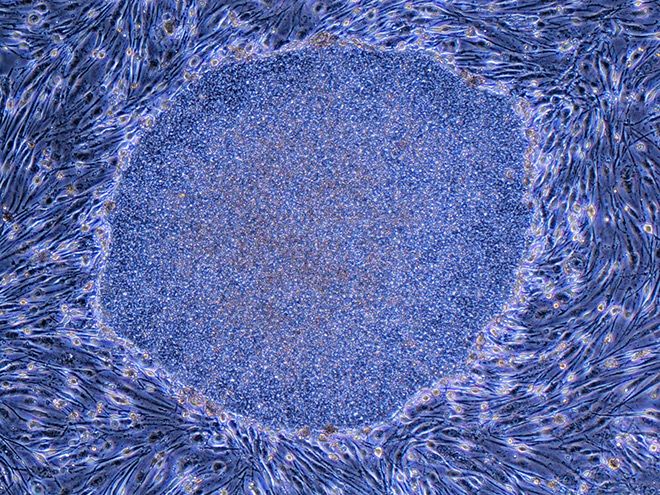
An expert panel at the health ministry greenlit the domestic manufacturing and marketing of two regenerative medical products that use induced pluripotent stem (iPS) cells on Feb. 19. The health minister will grant formal approval at a later date. When approved, they will be the world’s first practical medicines containing iPS cells, which can be re-engineered into other types, 20 years after Kyoto University professor Shinya Yamanaka created them from mice cells in 2006. ReHeart is one of the products and is a cardiac muscle sheet for treating severe heart failure that was developed by Cuorips Inc., a startup originating at Osaka University. The other is Amchepry, a neural cell drug developed by Sumitomo Pharma Co. for the treatment of Parkinson’s disease. Both products are made using third‑party iPS cells stocked by CiRA Foundation, which was established by Kyoto University. SMALL, BUT EFFECTIVE TRIALS ReHeart is intended for patients with ischemic cardiomyopathy, in which blood vessels become blocked due to conditions such as myocardial infarction or arteriosclerosis. Treatment using ReHeart involves converting iPS cells into cardiac muscle cells, forming them into a sheet and applying the sheet to the damaged area of the heart. The substances secreted from the sheet are meant to promote blood vessel regeneration and alleviate symptoms such as shortness of breath. Symptoms present during daily life improved one year after surgery in all eight patients who took part in its clinical trial. Four showed improved physical condition. Meanwhile, Amchepry is intended for patients whose dopamine levels in the brain have decreased due to Parkinson’s disease. In the treatment using the product, neural precursor cells derived from iPS cells are transplanted into the patient’s brain. The transplanted cells are expected to produce dopamine, thereby improving symptoms such as tremors in the limbs. In its clinical trial, symptoms improved in four of six patients two years after the transplant despite a diminishing response to other existing medication. It was confirmed that the transplanted cells remained in their brains, produced dopamine and that their overall dopamine levels increased. Approval was granted for both products under the “conditional and time‑limited approval system,” which is designed to deliver regenerative medicine products to patients as quickly as possible. This system serves as a provisional license, allowing safety and efficacy to be assessed using data from fewer patients than is required for conventional pharmaceutical clinical trials. Effectiveness only needs to be “presumed” to qualify. Because of this, companies are required to collect data from all cases in which the products are used during the seven‑year approval period. During the approval period, the aim is to use ReHeart with 75 patients and Amchepry in 35 patients. Thirty of the 35 patients for Amchepry must be 65 or younger. Based on the results, the companies must undergo another assessment on the products' effectiveness and other factors to obtain final approval. COVERED BY NATIONAL INSURANCE Even after the products receive approval from the health minister, it is expected to take several more months before they can be used in clinical settings. The earliest they are likely to become available is around summer, after drug pricing has been finalized. These products will be covered by the public health insurance system. The out-of-pocket burden on patients will also be kept low because the high‑cost medical expense benefit program is applicable. However, due to the high manufacturing costs, the drug prices are expected to reach several tens of millions of yen or more. In addition, they will be used only for certain patients at medical institutions equipped to properly handle cell‑based products and under the care of specialized physicians. Both products underwent only small clinical trials involving fewer than 10 patients to gain provisional approval. Safety and efficacy will need to be reassessed after the products are put on the market. Among the regenerative medicine products that have previously received such approval, there have been cases in which efficacy could not be confirmed, leading to discontinuation of sales or withdrawal of the application. Yamanaka, who was the co-recipient of the Nobel Prize in Physiology or Medicine in 2012 for his work with iPS cells, emphasized the value of reassessing products in a statement released on the Center for iPS Cell Research and Application’s website on Feb. 19. “I am very pleased that we have been able to take a major step toward social implementation in this milestone 20th year," he said. "To establish these treatments as medical practice, it is essential to verify their safety and efficacy in many more cases from here on.” (This article was written by Kazuya Goto, Shoko Tamaki and Kazuhiro Fujitani.)
Share this story